Choosing your maternity hospital
Which Singapore maternity hospital should I choose?

You will make plenty of decisions during pregnancy, and choosing where to deliver your baby is one of the most important ones to make. Most obstetricians are usually affiliated with one or more maternity hospitals, so it helps you narrow down your choices by asking your doctor which hospital they are affiliated with.
To make the best and most informed decision on which hospital to deliver, you can sign up for hospital tours to find out more about their amenities and services. As a guide, we have provided you with a summary of the private maternity hospitals in Singapore.
Gleneagles Hospital

Gleneagle’s packages start from $2,714 (two nights, normal delivery, GST inclusive) for a 2-bedded room. With their single-room packages (from $3,924 including GST), you can celebrate this joyous milestone with your loved ones with a celebratory tea set for 6. Daddies are also taken care of with meals and lodging during the hospital stay. Included within this value-for-money package are comprehensive newborn screenings and a personalised lactation consultation. They offer parking or a limousine service upon discharge as well. Gleneagles hospital is certified under the baby friendly hospital initiative (BFHI) to provide support to mothers in breastfeeding
The most luxurious room is the Dempsey suite, as pictured above. You can expect butler services, a customised VIP menu and additional offerings such as a romantic dinner for 2. The package for this suite starts at $10,024 (two nights, normal delivery, GST inclusive). For ease of mind, mommies can also look forward to a personalised breastfeeding coaching session with a professional lactation consultant and customisation of their confinement menu!
To find out more about Gleneagles’ maternity services and to take a virtual tour, visit www.gleneagles.com.sg/maternity.
Mount Elizabeth Novena Hospital (MENH)

After all the hustle and bustle, some mommies-to-be might want to welcome your little one in comfort and privacy. MENH is the only all-single-room hospital in Singapore and is also BFHI-certified. You will be welcomed with a mini bar, free wifi, and a 46-inch LED TV with an in-room entertainment system that includes a Parentcraft channel that screens breastfeeding education videos. MENH ensures that all of your needs are met, including meals and lodging for your accompanying family member. Their packages start at $4,062 (two nights, normal delivery) for single rooms, which includes a newborn hearing test and free parking for one vehicle during the package length of stay.
Mommies-to-be who are considering an upgrade to the junior suite can expect personalised breastfeeding coaching and a personalised newborn bath demonstration conducted by their experienced lactation consultant. MENH’s junior suite is priced from $9,393 for three nights for a normal delivery, which comes with an adjoining living room and an outdoor terrace and includes parking for two vehicles.
To find out more about Mount Elizabeth Novena’s maternity services and to take a virtual tour of the rooms, visit www.beststartinlife.sg.
Mount Elizabeth Hospital (MEH)

All maternity packages at MEH include customised confinement menus, a baby care and breastfeeding class, newborn health screening, hearing test, wifi, and parking for one vehicle during the package length of stay. For a regular single room, packages start at $3,970 (two nights, normal delivery, inclusive of GST). There is also two-bedded room option starting at $2,996 (two nights, normal delivery, inclusive of GST).
For a more lavish stay, the Daffodil and Magnolia Suites are specially designed to provide a luxurious setting that includes a spacious guest lounge to enjoy the delights of birth with your family and friends. The suites come with a butler, a personalised baby care and breastfeeding lesson, a limousine service upon discharge, and a baby metabolic screen and bilirubin test. Mommies can also enjoy a head-and-shoulder massage, a pampering hair spa, a manicure or pedicure while partners enjoy lodging and meals.
Parents can request a romantic dinner for two or mocktails for up to six guests to celebrate the birth of their child. The packages for one of these suites start at $12,741 (three nights, normal delivery, inclusive of GST).
To find out more about Mount Elizabeth’s maternity services and to take a virtual tour of the rooms, visit www.mountematernity.sg or call 6250-0000.
Parkway East Hospital (PEH)

At PEH, they try to give nursing care in a warm, supportive environment to women who are expecting. Apart from providing newborns with a comprehensive health screening, from blood screening to their first dose of vaccination, PEH also ensures that mothers get a supportive environment by offering complimentary Parentcraft classes to help you pick up nutrition tips for breastfeeding and advice on maternity confinement. Mothers also get a diaper bag with gifts and things they and their babies will need. Being BFHI-certified, PEH has lactation consultants to visit mothers to help them with breastfeeding.
Their packages for the single room start at $3,883 (two nights, normal delivery). Mothers will be served with a personalised postnatal confinement menu and fathers can select their meals from their wide range of choices!
To find out more about Parkway East’s maternity services, visit www.parkwayeast.com.sg.
Thomson Medical Centre (TMC)

If you’re looking for peace and space, the rooms at Thomson Medical Centre are designed to look like a contemporary resort setting with an understated luxury and spaciousness. The Thomson Family Suite comes with a dedicated team of staff, a separate living room area, free wifi, a mini fridge with a beverage corner, and daily newspapers.
The packages for a single single-bedded room start at $4,039.25* (two nights, normal delivery, inclusive of GST). There are also two- and four-bedded room options starting at $2,785.21* and $2,469.56*, respectively (two nights, normal delivery, inclusive of GST).
Find out more about the hospital tours at www.thomsonmedical.com or call 6358-0055 or 6350-8876. TMC’s diagnostics centre (TDUC) is located at Novena Medical Centre. When maternity tours resume after the COVID-19 situation, they are held Mondays to Fridays at 1pm, 2pm and 3pm, and Saturdays at 11am and noon.
*These rates are published from June 2020.
The best way to clear up any doubts you may have is to find out more with the help of the person in charge of the hospital tour. Cordlife is also located at MENH, PEH, and TDUC (TMC's diagnostic centre located at Novena Medical Centre). Drop by our consultation booths to find out more about how you can protect and safeguard your family’s health for a lifetime!
Recent Blog Posts
- 28 Mar 2025
- 10 Nov 2023
- 19 Oct 2022
- 19 Oct 2022
- 19 Oct 2022
Preparation for breastfeeding
Preparation for breastfeeding

Breast milk is the "best food" for your baby, and breastfeeding benefits mothers too. Breast milk has all the nutrients your baby needs to grow up healthy, like proteins, lipids, carbohydrates, vitamins, minerals, and other nutrients, in the exact amount she needs for her age. In the form of antibodies in your breast milk, you give your baby part of your immune defense when you breastfeed. This helps your baby's immune system because their natural defenses aren't quite ready yet.
Most of all, breastfeeding can heighten the bond between mother and baby.
Preparation for breastfeeding
Breastfeeding is a skill that may or may not come to you naturally in the beginning, but you will pick it up eventually once you get started. Therefore, it is important to prepare yourself mentally and physically for a good start.
Physical preparations

Having a well-balanced diet is important during pregnancy and after giving birth. Go shopping for nursing bras with good support and clothes (preferably 2-piece clothing) with roomy fitting for breastfeeding. If you have any doubts or worries about your physical condition, you can seek advice and help from a doctor by taking a breast examination.
Mental preparation

Read more about breastfeeding and the experiences that other mothers are sharing. Find out where you can look for help if needed. Most maternity hospitals have trained lactation nurses that you can call on for help regarding breastfeeding. You can also attend a breastfeeding talk with your partner to learn more.
Do think and plan how long you will breastfeed your baby so that you can make the necessary arrangements, especially if you are returning to work after your maternity leave. Check to see if your place of work has a nursing room or a private place for you to express milk, and let your boss know that you will need some time off to do this.
Most importantly, keep a positive mindset and be confident that you will succeed.
Recent Blog Posts
- 28 Mar 2025
- 10 Nov 2023
- 19 Oct 2022
- 19 Oct 2022
- 19 Oct 2022
What is cord blood banking and why you should consider it?
What is cord blood banking and why you should consider it?
The term “cord blood banking” has been heavily discussed among parents lately. But what is it exactly and what can it do for you and your family?
We have put together some information to help you understand exactly what it is.
Stem cells are essentially the building blocks of the human body. The umbilical cord, which serves as the lifeline between mother and baby for nine months, is an abundant source of these stem cells.
What is cord blood and cord lining banking?

Cord blood, also called “placental blood”, is blood that remains in the umbilical cord and placenta following the birth of a baby and after the umbilical cord is cut after delivery.
Cord blood banking is the process of storing your child’s umbilical cord blood, which is a rich source of stem cells should the need for a stem cell transplant ever arise.
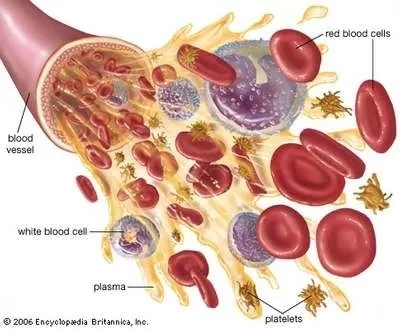
Cord blood is particularly rich in haematopoietic stem cells (HSCs), which are responsible for replenishing the blood and regenerating the immune system. HSCs are known as "precursor cells’ as they have the unique ability to differentiate into the different types of cells found in the body, namely:
- Red blood cells – to transport oxygen throughout the body
- White blood cells – produces antibodies and fights infections
- Platelets – assists in blood clotting
Haematopoietic stem cells, or HSCs have been used to treat over 80 diseases such as leukaemia, lymphoma, and thalassaemia, as well as metabolic and immune disorders.1 Clinical trials are also underway to use cord blood for the treatment of autism, cerebral palsy, type 1 diabetes, Alzheimer’s disease, spinal cord injury, and many more.2 Clinical trials are one of the main ways that medical advances happen, and they give hope to families whose loved ones have diseases that have no known cure.
Other than cord blood, there is also a sheet-like membrane surrounding the umbilical cord, known as the cord lining. The cord lining contains an abundance of mesenchymal stem cells (MSCs) and cord lining epithelial cells (CLECs), which are the “muscle-forming” and “skin-forming” building blocks in the human body. Both MSCs and CLECs have shown potential in aiding the repair of injured tissues and organs, as well as the treatment of various diseases.
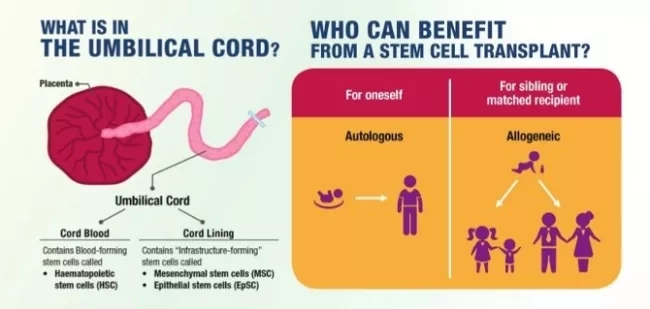
Since cord lining stem cells can change how the immune system works, it is easier to find a match between a donor and a patient. This makes them a good choice for both your baby and other members of your family. Although the medical use of cord lining stem cells is still under clinical trials, the list of potential treatments includes stroke, heart failure, Alzheimer’s disease, Parkinson’s disease, spinal cord injury, and type 1 diabetes, just to name a few.
While different types of stem cells serve varying functions, when used in tandem, they can work in synergy to help speed up the treatment process by promoting the growth of healthy cells and reducing immune system complications.
By storing a combination of HSCs, MSCs and CLECs, you are enabling your children and family to be part of a medical revolution with access to the growing applications of stem cells and the therapeutic potential they hold.
Why should I save my baby’s cord blood?

Data has shown that there is an increasing likelihood of using HSCs for medical treatments as one ages. With statistics also showing that 1 in every 217 people may require a stem cell treatment in their lifetime, storing your baby’s cord blood gives you the assurance of having a ready source of HSCs, should a time-critical situation ever arise.3 While it is possible to do a national or international search, the process can be both costly and time-consuming. Furthermore, the odds of finding a match for a transplant within the same racial group are around 1 in 20,000.4
There are also other sources of stem cells, such as those from a matched bone marrow donor and peripheral blood. However, the advantage of using cord blood stem cells is that they’re younger and more primitive, meaning these cells are faster in generating healthy cells and are also more tolerant to tissue mismatches, which may happen in transplants involving a donor.
Advantages of using cord blood over other sources:
| Source | Bone Marrow | Peripheral Blood | Cord Blood |
|---|---|---|---|
| Collection | Multiple extractions | Needs multiple growth-hormones injections | Quick, painless & risk-free for both mother and child |
| Type of stem cell | Adult | Adult | Perinatal* |
| Availability | Donor search | Donor search | Readily available (for family bank) |
| Graft vs Host Disease | High Risk | Higher risk | Minimal risk |
| Cost of obtaining a matching unit | Can cost up to S$64,000 | Can cost up to S$64,000 | $0 (100% ownership for family cord blood bank |
*Definition of perinatal: pertaining to the period immediately before and after birth
By storing your baby’s precious cord blood, you are giving him/her ready access to his/her life-saving stem cells should the need for a stem cell transplant ever arise. As a baby’s cord blood is a 100% match for him/her, it is a guaranteed match for autologous transplants (where the donor and the recipient are the same individual) with no risk of post-transplant rejection.
If there is a suitable match, his/her cord blood may also be used for an allogenic transplant (in which the donor and recipient are different people) for his/her siblings or family members. Studies have shown that the overall 3-year survival rate for patients who got cord blood from a relative was 95%, while it was only 61% for patients who got cord blood from someone else.5
How do you choose the right family cord blood bank?
Given the current and potential value that the stem cells in your baby’s cord blood hold, it’s important to choose the right family cord blood bank that you trust and know will be with you for the long haul. Here are some key factors to consider when it comes to choosing the right family cord blood bank to store your baby’s life-saving umbilical cord stem cells
Long-standing establishment
A family cord blood bank that has been around for a long time gives parents peace of mind that their child's valuable cord blood stem cells are being kept by a trustworthy partner who will be there for the long haul. With over 22 years of experience and establishment in Singapore, Cordlife is the 1st and largest family cord blood bank in Singapore.

Accreditations
Choose a family cord blood bank that has been accredited by independent international bodies. The Parent’s Guide to Cord Blood Foundation, an educational resource for parents, recommends selecting a family cord blood bank that is accredited by international bodies such as the Association for the Advancement of Blood & Biotherapies (AABB).6
These accreditations ensure that the family cord blood bank adheres to the highest standards of quality when it comes to the handling, processing, and storing of cord blood through regular and rigorous audits. It also ensures that your child’s cord blood stem cells will still remain viable should the need for transplantation ever arise.
Transplant track record
Another important factor to consider is whether the family cord blood bank has a proven track record of releasing cord blood for transplants. A family cord blood bank with a proven track record and experience in successfully releasing cord blood for transplants is an indication that the cord blood stem cells are being stored according to the highest standards and will still be viable for transplantation.
Unique service offerings
Find out if the family cord blood bank has other services to offer, as it means that you will be able to maximise the medical options for your child and family members.
Apart from storing cord blood stem cells, Cordlife is the sole provider of umbilical cord lining storage in Singapore and is also one of four family cord blood banks worldwide licensed to store an additional two types of stem cells-mesenchymal stem cells (MSCs) and cord lining epithelial cells (CLECs).
This increases your child and family’s medical options for possible therapeutic and regenerative applications in the future, especially for conditions that currently have no known cure.
Facility
A family cord blood bank that owns its own processing and storage facility is able to maintain direct control over critical services, quality, licensing, and accreditation, thereby ensuring the well-being of the families whose cord blood units are stored under its care. It also lets the family cord blood bank use its resources right away in case of an emergency. Cordlife has over 22 years of experience and lab management expertise.
Financial stability
Deciding to store your baby’s precious cord blood is a long-term decision. Public listed companies offer financial transparency for increased assurance.
As storing your child’s cord blood stem cells is a life-saving investment, it’s important to ensure that the family cord blood bank is financially stable, has a good reputation, and has many years of operation and experience. This is to ensure that they will be with you and your family for the long haul.
Some other factors to take note of also include the family cord blood bank’s processing technology, customer service, and enrolment process, just to name a few.
Setting aside a budget to store your baby’s cord blood is a smart investment, but it will be a futile one if you pick the wrong family cord blood bank to safeguard it. So, be diligent in researching the family cord blood bank’s certifications, reputation, facilities, and technologies used to process and store your child’s cord blood unit, and you will be on your way to making a lifesaving investment for the future.
Written by Mummy Mylene
1Diseases Treated page. Parent’s Guide to Cord Blood Foundation website. https://parentsguidecordblood.org/en/diseases. Accessed July 16, 2018.
2Diseases and Disorders that have been in Clinical Trials with Cord Blood or Cord Tissue Cells page. Parent’s Guide to Cord Blood website. Therapies in Clinical Trials. https://parentsguidecordblood.org/en/diseases#trial. Accessed July 16, 2018.
3Nietfeld JJ, Pasquini MC, Logan BR, et al. Lifetime probabilities of haematopoietic stem cell transplantation in the U.S. Biology of Blood and Marrow Transplantation. 2008; 14: 316-322.
4Chew J. Criterion for new stem-cell transplant 50% match. The Straits Times. July 18, 2013: 12-15.
5Bizzetto R, Bonfim C, Rocha V, et al. Outcomes after related and unrelated umbilical cord blood transplantation for hereditary bone marrow failure syndromes other than Fanconi anemia. Haematologica. 2010; 96(1):134-141.
6Frequently Asked Questions page. Parent’s Guide to Cord Blood website. https://parentsguidecordblood.org/en/faqs#q-18082. Accessed July 16, 2018.
This article was adapted from SuperMom, 25 August 2018.
Recent Blog Posts
- 28 Mar 2025
- 10 Nov 2023
- 19 Oct 2022
- 19 Oct 2022
- 19 Oct 2022
Guide to maternity costs for expectant parents
Guide to maternity costs for expectant parents
Congratulations on your bundle of joy!
It’s known that having a child requires some form of financial planning and resources, as the financial cost of raising a child starts even before the child is born.
The cost of having a baby in Singapore depends on a number of factors, such as the hospital, the gynaecologist package, and the way the baby is born.
Here’s a guide on the key cost components that you should expect from a baby bump to delivery!

Recent Blog Posts
- 28 Mar 2025
- 10 Nov 2023
- 19 Oct 2022
- 19 Oct 2022
- 19 Oct 2022
High blood pressure in pregnancy
High blood pressure in pregnancy
By Dr. Jonathan Wee
Consultant Obstetrician and Gynaecologist
MBBS (S'pore), MRCOG (UK) M MED (O&G) (S'pore), FAMS (O&G)
What you need to know to protect yourself and your baby
High blood pressure, or hypertension, can be present in a few different ways during pregnancy. It's one of the most common health problems during pregnancy, causing problems in up to 15% of cases. If you have or develop high blood pressure in pregnancy, you are likely to require special care during your pregnancy and should go for regular follow-up with your obstetrician. Here are some facts that you need to know to take care of yourself and your baby.

What are the different types of high blood pressure during pregnancy?
1. Chronic Hypertension
Chronic hypertension is high blood pressure (usually more than 140/90 mmHg) that was present before pregnancy or shows up in the first 20 weeks of pregnancy. It usually carries on after delivery.
2. Gestational Hypertension
Gestational hypertension (or pregnancy-induced hypertension) is high blood pressure that develops after 20 weeks of pregnancy without significant protein in the urine or other signs of organ damage. This transient hypertension usually goes away after delivery.
3. Preeclampsia
This is a serious condition in pregnancy which can arise from both chronic hypertension and gestational hypertension. Symptoms include high blood pressure and protein in the urine, and it is occasionally associated with other signs of organ damage. Left untreated, it can give rise to serious complications for both mother and baby.
What are the problems with regards to high blood pressure in pregnancy?
Untreated or poorly controlled hypertension or preeclampsia in pregnancy can lead to serious risks.
1. For the mother
Mothers can be at risk of damage to their kidneys and liver, stroke, blood clotting problems, as well as bleeding from the placenta. There is also the risk of preeclampsia leading to eclampsia, which is an acute and life-threatening complication that is characterized by seizures and possibly coma in pregnancy.
2. For the baby
Your foetus can be at risk of poor growth, an increased risk of premature delivery and stillbirth, and premature separation of the placenta from the inner wall of the uterus before delivery, also known as placental abruption.
Who is more likely to develop high blood pressure in pregnancy?
Here are some of the risk factors for developing high blood pressure in pregnancy and preeclampsia.
- Women in their first pregnancy
- Women who had high blood pressure or any hypertensive disease in a previous pregnancy
- Women with a first degree relative who had high blood pressure in pregnancy
- Women with twins or other multiple pregnancies
- Women above the age of 40 or under 20
- Women who are overweight
- Women with chronic kidney problems or diabetes
- Women whose last pregnancy was over 10 years ago

Recent Blog Posts
- 28 Mar 2025
- 10 Nov 2023
- 19 Oct 2022
- 19 Oct 2022
- 19 Oct 2022
Clearing the misconceptions: pain relief in labour
Clearing the misconceptions: pain relief in labour
By Dr. Arthur Tseng
Consultant, Obstetrician and Gynaecologist, Urogynaecologist
MBChB (Sheffield), MRCOG (UK)

For countless women, the joy of pregnancy is also intermixed with a fear of labour and the pain that is necessary for delivery. This fear is compounded by all the horror stories of labour pain-relief methods that do not work, or worse still, cause unpleasant or dangerous side effects and complications. This article will attempt to dispel certain myths and allay fears that there are good and effective methods of pain-relief for labouring women.
When will you start experiencing labour pain?
As the pregnancy approaches term, which is defined as 37 completed weeks of gestation, the womb (uterus) starts to contract. What were previously painless Braxton-Hick contractions ends with transition to painful labour contractions. Initially, these contractions are irregular but progressively become regular and more intense. In women with their first pregnancy, regular contractions happen about once every 10 minutes. In women with their second pregnancy or later, regular contractions happen about once every 15 minutes or in shorter cycles. Typically, the cervix will be dilated to three to four centimetres in diameter. The water bag may also rupture, causing leakage of amniotic fluid; and there may be a "show" where the mucus plug is dislodged from the dilating cervix, accompanied by blood.
Stages of labour
In the first stage of labour, the cervix opens up from 3 to 10 centimetres. This can take 8 to 10 hours for a first-time mother and, on average, 4 to 6 hours for a woman with more than one child. In the second stage of labour, when the baby is born by pushing in time with contractions, it can take up to two hours for a woman who has never given birth before and up to an hour for a woman who has given birth before. After delivery, cord blood banking may be performed, and active management of the third stage of labour reduces the risk of severe bleeding (post-partum haemorrhage). This entails delivering the placenta by controlled cord traction, manually rubbing the uterus to cause a sustained contraction , and various medications to stop bleeding. Most women want to breastfeed their babies exclusively, and the team in the delivery room would encourage this right away, along with skin-to-skin contact to help the mother and her baby bond.

It would appear that labour does take a certain length of time, during which there will be regular contraction pains to contend with. Pain is debilitating when it occurs repetitively; it saps our concentration and strength. It also causes various bodily changes in the labouring mother, increasing the workload of the mother’s heart, increasing blood pressure, reducing placental blood flow and causing uncoordinated uterine contractions, thus leading to prolonged labour and a greater chance of foetal distress. As such, any method of blocking labour pains would intuitively improve maternal and foetal outcomes and likely shorten the duration of labour.
How to manage labour pain?
There are non-pharmacological and pharmacological methods of reducing or blocking labour pains. In terms of non-pharmacological pain-reducing methods, one of the most useful is that of continuous labour support. Someone there to help the labouring mother, like a partner or spouse, a relative, a nurse on staff, or a midwife, has been shown to shorten the length of labour, decrease the number of times the mother asks for painkillers, improve the overall labor experience, and decrease the number of times she needs an assisted instrumental delivery or a Caesarean section.1 Other methods that appear to work are acupuncture, hypno-birthing, and water baths. Acupuncture does relieve pain, thus reducing the need for pharmacological analgesics. It is safe if performed by an expert. Hypno-birthing does reduce the need for further analgesics and improves the overall birthing experience. Water baths can temporarily ease pain and muscle spasms, and they don't raise the risk of foetal distress. Hence, it is considered safe for a labouring mother to have a warm bath.2 Massage therapy, touch therapy, certain birthing positions for the mother, aromatherapy, audial analgesia, and Transcutaneous Electrical Nerve Stimulation (TENS), which is supposed to ease pain by stimulating nerves with an electronic device, have not been shown to work.
In hospitals, all maternity wards and delivery rooms have the tools and services needed for effective pharmacological pain relief. There are currently three available: Entonox gas analgesia, Pethidine injections, and Epidural analgesia. They have varying effectiveness and are suitable for different occasions, and the effectiveness can be quantified by using a Wong-Baker visual analogue scale (VAS) system – where a pain-score of ‘0’ is completely pain-free, and ‘10’ would be the worst possible pain experienced by an individual.
Entonox is considered the mildest of the three pharmacological pain-relief methods. Entonox is a mixture of nitrous oxide (laughing gas) and oxygen. The combination of gases does provide mild analgesia from labour pains. To get the most out of Entonox, women in labour do have to time when they breathe it in with the start of a contraction. As Entonox stays in the body system for only as long as the gas is inhaled, analgesia wears off rapidly once room air is inhaled. As such, Entonox is very safe for the mother and the unborn baby, as well as the healthcare workers in the delivery suite.4 When used to control labor pain, Entonox effectively reduces the pain score by 1 to 2 points.
Intramuscular (IM) Pethidine injection is another common painkiller. It is made from opium and has been used since the 1970s. Both nursing and medical personnel can administer Pethidine every 4 to 6 hours. Opium-derived analgesia causes nausea and vomiting; as such, an anti-nausea agent is usually given at the same time (IM Maxalon or Stemetil) as a preventative agent. Pethidine injections can be given more than once, but this causes the drug to build up in the body. It is also not a good idea if the baby is about to be born soon, since the highest concentrations in the foetus are found 2 hours after the injection. This can lead to a risk of sedation in the newborn, which may require neonatal resuscitation.5 When used during labour at appropriate times, pethidine effectively reduces the pain score by 4 to 5 points.

Epidural analgesia is currently used extensively for labour pain management, and involves the introduction of local anaesthetic solution into the space surrounding the spinal cord nerves (the epidural space), to produce markedly diminished or absent pain perception, via a fine and flexible plastic tube, that is inserted by an anaesthetist. It is effective in reducing pain scores by 8 to 9 points. Frequently, labouring women are completely pain-free after an epidural, compared to other simpler forms of analgesia, and they can still opt for an epidural if the side effects of other medications are intolerable, or if their labour is advanced and Pethidine cannot be administered safely.
Women with medical conditions also benefit from an epidural. Women with high blood pressure or pre-eclampsia have better control of their blood pressure during labour, and the blood flow to the placenta is better, which makes it less likely that the baby will be in distress during labor and delivery, especially if the baby is small. Diabetic mothers and women with gestational diabetes have a better time keeping their blood sugar under control during labour. With the right pain relief, they can also have smooth instrumental deliveries or Caesarean sections if they need to. In cases of twin pregnancy, breech babies, and vaginal birth after caesarean (VBAC), there is a higher risk of conversion to caesarean section, and an epidural facilitates a smooth transition from labour to caesarean when required.6 Patients with clotting problems due to medical conditions, back skin infections, spinal problems, a history of spinal surgery, and severe cardiac disease are not suitable candidates for an epidural.
Side effects of epidural
When one uses an epidural, one of the commonest side effects experienced is numbness and weakness of the lower body and legs due to a variable degree of motor nerve block. Other side effects commonly felt are nausea and vomiting, shivering, transient blood pressure changes, and difficulty with passing urine. Hence, many patients have an indwelling catheter inserted once they are on an epidural. Other uncommon side effects are those of inadequate pain relief; a one-sided block (where the patient experiences pain on one side of the body and not the other); and rapid progression of labour, such that the labour process is shortened dramatically, and delivery becomes imminent. Rarely, there are very serious side effects like seizures and respiratory arrest.
Aside from the side effects, there are some myths about what an epidural is and how it works. One such myth is that epidurals can result in long-term backaches. Another such myth is that epidurals may potentially harm the baby, or increase the risk of Caesarean section, and that epidurals cannot be used too early in labour.
It was found that 53 to 89% of pregnant women experience back pain during their pregnancy. Instead, the pain was caused by physiological changes associated with pregnancy, such as poor posture, spinal anatomical changes associated with pregnancy, hormonal changes resulting in ligament relaxation and water retention, all of which contribute to additional ligamentous laxity.7 Obstetricians say it's a good idea to go back to your old exercise routines, especially core body strengthening exercises, after giving birth to lower the risk of long-term back pain.
When should epidural be administered?
In one study, there was a comparison between epidurals given early before established labour had started and epidurals given later in established labour. It was found that patients who got an epidural early (when the cervix was less than 4 centimeters open) had shorter labours and didn't have a higher chance of needing a Caesarean section. It was also found that the babies delivered had better health assessment scores (Apgar scores), apart from superior pain relief. 8 It is thought that when a woman isn't in pain, her pelvic floor muscles relax, making it easier for the baby to move through the birth canal. This may be why labour shortages happen. It was found that using an epidural was linked to a better neonatal acid-base balance status. This is a way to measure peri-partum health, and it again suggests that using an epidural during labor keeps the placenta oxygenated and nourished for the baby.9

Many women don't like being in labour, and it shouldn't be okay for them to be in pain that can be eased with safe and quick methods of analgesia. It is said that a mother's request for pain relief during labor is a good enough reason to give it if there is no medical reason not to.10 So, knowing what kinds of pain relief are available and the pros and cons of each one helps patients feel more comfortable and, just as importantly, safer during labour, for both the mother and the baby.
References:
1) Simikin et al. Systemic review of 5 non-pharmacological methods of pain relief during labour. Am J Obstetrician Gynaecol 2002.
2) Smith et al. Complementary and alternative therapies for labour pain. Cochrane Database 2006.
3) Carroll et al. TENS does not relieve labour pain: a systemic review. Contemporary Reviews in O&G, 1997.
4) Rosen MA. Nitrous Oxide for labour pain, a systemic review. Am J OG 2002.
5) Briker et al. Parenteral opioids for labour, a systemic review. Am J OG 2002.
6) Reynolds et al. Analgesia in labour and acid-base balance: a meta-analysis comparing epidural with systemic opioid analgesia. BJOG 2002.
7) Lim, et al. Dispelling the myths of epidural relief in childbirth. SMJ 2006; 47(12):1096.
8) Wong CA, et al. the risk if caesarean delivery with neural oak analgesia given early versus late in labour. The NEJM 2005; 352(7).
9) Reynolds F, et al. Analgesia in labour and foetal acid-base balance: a meta-analysis comparing epidural with systemic opioid analgesia. Br J Obstetrician Gynaecol (BJOG) 2002.
10) ACOG Practice Bulletin No. 36: Obstetric Analgesia and Anaesthesia. Obstetrics & Gynaecology 2002; 100(1): 177-191.
Recent Blog Posts
- 28 Mar 2025
- 10 Nov 2023
- 19 Oct 2022
- 19 Oct 2022
- 19 Oct 2022
Vomiting in early pregnancy: when it isn't normal
Vomiting in early pregnancy: when it isn't normal
By Dr. Goh Shen Li
Obstetrician & Gynaecologist
MBBS, FRCOG (London), FAMS (Singapore)
The majority of pregnant women experience some degree of nausea and vomiting (70–80%) in the first trimester of pregnancy. Its severity can vary from person to person and even during different pregnancies in the same woman.
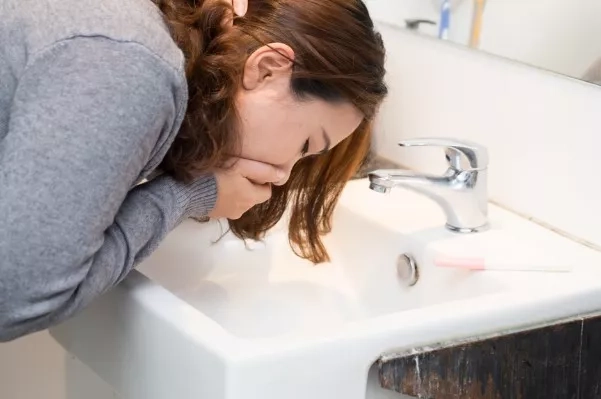
When the vomiting is severe
Hyperemesis gravidarum (HG) is a condition in pregnancy characterized by extreme nausea, excessive vomiting, weight loss and dehydration, and even fluid and electrolyte imbalances. It affects up to 2–3% of pregnant women.
People don't get HG very often, but nausea and vomiting are common during pregnancy, so it can be hard to tell the difference between this and the more common pregnancy sickness. (PRODIGY 2008, Festin 2009, HER 2010, Matthews et al 2010, Ogunyemi and Fong 2009) HG usually begins at between 6 and 7 weeks of pregnancy (HER 2010), easing off at 14 to 16 weeks of pregnancy. In many cases, HG will end by 20 weeks of pregnancy. Very few sufferers have symptoms that last the whole pregnancy.
How do I know if this is normal or not?
If you have HG, self-help treatments cannot help much and you feel miserable. You are exhausted and are unable to enjoy the pregnancy. You struggle with day-to-day life and are unable to eat and drink. You find it difficult to swallow your own saliva without vomiting (Ogunyemi and Fong 2009, Suzuiki et al. 2009, HER 2010). You vomit several times a day, and you are losing weight.
Recognise the following signs and symptoms - (HER 2010)
- Loss of 5% or more of pre-pregnancy body weight
- Dehydration, causing metabolite disturbances and constipation
- Nutritional disorders such vitamin deficiencies
- Physical and emotional stress of pregnancy on the body
- Difficulty with activities of daily living
- Severe nausea and vomiting
- Food aversions
- Decrease in urination
- Headaches
- Confusion/ fainting
- Jaundice
- Extreme fatigue
- Low blood pressure
- Rapid heart rate
- Loss of skin elasticity
- Secondary anxiety/depression
Hunger, tiredness, prenatal vitamins (especially those with iron), and diet can all make symptoms worse. Some women with HG lose as much as 10% of their body weight. They are also very sensitive to smells around them, and some smells can make their symptoms worse.
| Morning Sickness: | Hyperemesis Gravidarum: |
| Nausea sometimes accompanied by vomiting | Nausea accompanied by severe vomiting |
| Nausea that subsides at 12 weeks or soon after | Nausea that does not subside |
| Vomiting that does not cause severe dehydration | Vomiting that causes severe dehydration |
| Vomiting that allows you to keep at least some food down | Vomiting that does not allow you to keep any food down at all |

Why does this happen?
There are theories that suggest HG is due to a combination of factors, which may vary among women and include genetics, body chemistry, and overall health.
One theory is an adverse reaction to the hormonal changes of pregnancy. This would explain why HG happens most often in the first trimester (often between 8 and 12 weeks of pregnancy), when the levels of the pregnancy hormone (hCG) are the highest. Another postulation is an increase in maternal levels of female hormones in the body, leading to slower digestion and delayed passage of food from the stomach to the intestines, thus increasing the nausea and vomiting.
Risk factors for HG
- Hyperemesis gravidarum during a previous pregnancy
- Being overweight
- Having a twin pregnancy
- Being a first-time mother or young mother
- Being prone to motion sickness or migraines
- Pre-existing liver disease
- The presence of trophoblastic disease, which involves the abnormal growth of cells inside a woman's uterus e.g. molar pregnancy
Will my baby be in danger?
HG is physically and emotionally stressful, but it is also important to know that if it is treated, it is extremely unlikely that your baby will be malnourished or harmed (PRODIGY 2008, Festin 2009). Most studies show no health or developmental differences between infants of women who experienced the condition and those who did not.
If you lose weight during your pregnancy, there is an increased risk that the birthweight of the baby may be less than average. However, almost all women regain the weight they had lost in the early stages of pregnancy, usually during the second trimester, and go on to put on enough weight by the time of delivery.
Management of HG - what can be done?
- There is no known prevention of HG but you can take comfort in knowing that there are ways to manage it. All drugs should be used with care in pregnancy, especially in your first trimester, but many anti-nausea medications have a good safety record and have not been shown to have ill-effects on babies (PRODIGY 2008). Consider asking your doctor for anti-nausea medications to help you cope.
- Mild cases are treated with dietary changes, rest and oral medications. More severe cases often require a stay in the hospital so that the mother can receive fluid and nutrition through an intravenous line (IV).
Treatment depends on how ill a woman is and might include:
- Trying vitamin B6, and/or ginger.
- Small frequent meals—Nausea and vomiting might be treated with dry foods (such as crackers), small frequent meals and emotional support.
- Intravenous (IV) fluids—It is important for a pregnant woman to maintain her fluid intake. IV fluids might be needed if a woman continues to vomit throughout the pregnancy or does not improve with oral medications. In severe cases, hospitalisation is required for continued IV fluids and vitamins can be added into the IV fluids. IV fluids might be discontinued when a woman is able to take in fluids by mouth.
- Medicines — Medication to reduce nausea is used when vomiting is so persistent that it may pose possible risks to the mother or baby. If a woman cannot take medicines by mouth, the drugs can be administered through an IV or a rectal suppository. Common medicines used to alleviate nausea include promethazine, metoclopramide, prochlorperazine, and dimenhydrinate. If you are also heaving gastric reflux, anti-reflux medications can be given together as well. (HER 2010)
- Doing urine and blood tests to monitor the degree of dehydration and electrolyte levels e.g. sodium and potassium, and if abnormal, corrected with supplementation.

What next?
After IV rehydration is completed, you can progress to frequent small liquids or bland meals. Treatment then focuses on managing symptoms to allow normal food intake. However, cycles of dehydration can recur, making continuing care or repeated hospitalization necessary. (NHS 2010)
- Stay hydrated by taking small sips of fluid, or by sucking ice cubes (NHS 2010) or lollipops.
- Eat whatever you can manage or like. Do not worry if it is not a balanced diet or your regular meal. You can always catch up on good nutrition later, as your baby will get her nourishment from your body’s current reserves.
- Tweaking your diet to eliminate fatty and spicy foods, which are more likely to cause nausea
- Avoiding smells or tastes that tend to set you of.
- If you do not have severe anemia, wait until the nausea has improved before starting iron supplements.
- Try natural remedies such as ginger and peppermint alongside medical treatments (NCCWCH 2008, Festin 2009)
- Get as much rest as you can. Tiredness can make nausea and vomiting worse (NHS 2010), and make you feel unable to cope with the pregnancy. (PRODIGY 2008)
Recent Blog Posts
- 28 Mar 2025
- 10 Nov 2023
- 19 Oct 2022
- 19 Oct 2022
- 19 Oct 2022
The gift of life
The gift of life
By Dr. Choo Wan Ling
Consultant, Obstetrician & Gynaecologist
MBBS (Singapore), M.Med (O&G), FAMS

From conceiving to delivering
Having a baby is truly remarkable. From mutual love that creates new life, to the very first kick in your belly, and ultimately to the climacteric birth of your baby, the journey is nothing short of a miracle. While your joy is immense, it is only natural to have concerns at any point during this life-changing experience. For instance, you may be anxious to conceive or be apprehensive about childbirth.

Difficulty in conceiving: are there simpler treatments before in-vitro fertilization (IVF)?
As a woman ages, her chances of conceiving are slimmer, particularly above the age of 35.
For women, the common causes of infertility include ovulation problems, blocked or unhealthy fallopian tubes, and endometriosis.
For men, problems with hormones and genes, heavy smoking, varicocele, and infections can all cause sperm to be missing, too few, or not work right.
Treatment would involve resolving the abnormalities and individualising therapies to obtain the simplest, cheapest, and safest modality with reasonable success.
Options would include:
- Better understanding of the fertile period
- Knowledge and timing of the fertile period is essential, coupled with frequent sexual intercourse. Timed sex with ovulation – predicted from urine tests and a good menstrual calendar – may improve conception rates.
- Treating underlying hormonal disorders
- 80-90% of women achieve ovulation once hormonal abnormalities are corrected, increasing the chance of conception
- This can be achieved with fertility drugs ranging from oral medications to injections to boost ovulation.
- Intrauterine insemination
- Chances of conception can be further improved with intrauterine insemination in cases where there is mild sperm defect. This is a simple procedure where washed sperms are flushed into the womb at the time of ovulation.
- Corrective surgery
- Depending on the damage to the fallopian tubes, tubal surgery may be helpful. Success of pregnancy following tubal surgery is variable. Compared to IVF, surgery is a one time treatment with a higher potential for long term fertility. Surgery in endometriosis improves fertility rates but not back to normal levels.
- IVF
- Simpler options should be considered first before IVF but it may be needed for severely damaged fallopian tubes, significant endometriosis and considerable sperm abnormalities. Concerns surrounding IVF include cost, psychological, emotional and physical stress, higher risk of multiple pregnancies and premature birth.
Successful conception hinges on a myriad of factors concerning both partners. Do talk to a doctor if you and your partner have been having regular, frequent, unprotected sex for a year and still can't get pregnant.

Is my baby normal?
With increasing educational and socio-economic status, there is a trend towards deferred child bearing. The problems associated with late maternal pregnancy include maternal and fetal problems.
Firstly, there is an increased risk of miscarriage. There is also an increased risk of chromosomal abnormalities. The most common chromosomal abnormality is Down’s syndrome, which can be screened for in all pregnant women.
This screening test can be done between 11 and 13 weeks of pregnancy via a blood test and an ultrasound scan to measure the neck fold thickness and look for the nasal bone. It does not carry any risks to the fetus. This allows mothers the time to make an early choice about the pregnancy should an abnormality be detected. Confirmatory tests for Down’s syndrome include amniocentesis, which can be performed between 16 and 20 weeks of gestation, or chorionic villus sampling, which can be performed from the 11th week. Both confirmatory tests, however, are associated with a small risk of miscarriage.
Medical conditions like gestational diabetes and hypertension are more common in older mothers. Older mothers may also tend to have more problems in labour.
Even though having a baby when a mother is older poses more risks to the pregnancy, these risks can be managed by keeping a close eye on the mother during pregnancy and labor to reduce the chances of complications.
Recent Blog Posts
- 28 Mar 2025
- 10 Nov 2023
- 19 Oct 2022
- 19 Oct 2022
- 19 Oct 2022
Pregnancy and dental health
Pregnancy and dental health
By Dr. Tan Su Wee
While it is an old wives' tale that calcium is lost from a mother's teeth and "one tooth is lost with every pregnancy", changes experienced in your oral health during pregnancy may dramatically affect the way your dentition looks, feels, and functions. This is chiefly due to a surge in hormones; particularly an increase in oestrogen and progesterone, which can exaggerate the way gum tissues react to plaque.

How does a build-up of plaque affect me?
Poor oral hygiene results in a steady accumulation of plaque. The bacterium it brings about irritates our gum tissues, causing gum disease. In pregnancy, the effects of gingivitis are more pronounced. “Pregnancy gingivitis” causes red, swollen, tender gums that are more likely to bleed. Also, gum disease moves faster from gingivitis to periodontitis, which is an advanced form of gum disease that causes damage to our teeth and their supporting structures that can't be fixed.
Pregnancy Gingivitis might surface as early as the second month of pregnancy and can lead to significant discomfort and pain. Potential gum problems should be combatted with meticulous cleaning habits.
Pregnant women are also at risk for developing pregnancy epulis, an inflammatory, non-cancerous fleshy growth that develops when swollen gums become irritated. They do not usually require treatment and will shrink on their own after delivery. However, if it interferes with chewing, brushing, or other oral hygiene procedures, your dentist may decide to remove it.
How can I prevent these problems?
Brush with fluoride toothpaste twice daily and floss thoroughly. If you experience morning sickness and bouts of frequent vomiting, rinse your mouth with fluoride mouthwash followed by a generous application of re-mineralising tooth mousse afterwards to prevent erosion of your tooth structure. These products are available at your dentist. Regular checks (each trimester) and cleanings at the dentist during the 2nd trimester will also help control plaque, prevent gingivitis, and detect dental problems early. Good nutrition—particularly plenty of vitamin C and B12—will help keep the oral cavity healthy and strong.
When should I see my dentist?
If you are planning to become pregnant, schedule a routine check with your dentist. He/she will assess your oral condition and treat all dental problems prior to pregnancy.
If you are pregnant, make sure to let your dentist know prior to any dental visit. It is best to have a routine visual exam every trimester to check for any problems and to clean during the second trimester of your pregnancy. This is because the first three months of pregnancy are thought to be of the greatest importance in your child's development. Stress associated with dental visits may increase the incidence of prenatal complications during the last trimester.
Inform your dentist of all the names and dosages of drugs you are taking, including medications and prenatal vitamins prescribed by your doctor. Any specific medical advice your doctor has given you should also be communicated. Your dentist may need to alter your dental treatment plan based on this information. Certain drugs, such as tetracycline, can affect the development of your child's teeth and should not be given during pregnancy.
Do not skip routine dental checks because you are pregnant. Because of the way hormones change during pregnancy, it's important to get regular periodontal (gum) exams to stop gum problems from getting worse quickly. Pay particular attention to any changes in your gums during pregnancy. If tenderness, bleeding, or gum swelling occurs at any time during your pregnancy, seek help from your dentist as soon as possible.

Are there any dental procedures I should avoid?
The best time for routine dental treatment is the fourth through sixth months. Dental emergencies that cause a lot of pain can be treated at any point during a woman's pregnancy. However, your obstetrician should be consulted if you need anaesthesia or if you are given medicine. Treatments that aren't necessary, like getting your teeth whitened or getting other cosmetic work done, should wait until after the baby is born. It is best to avoid cosmetic dental work while pregnant to keep the developing baby from being exposed to any risks, no matter how small.
Routine x-rays (radiographs) taken at yearly intervals to screen for cavities should be postponed until after birth. In certain dental emergencies, such as extractions, radiographs might be necessary for diagnosis and treatment of the pregnant patient. According to the American College of Radiology, no single diagnostic x-ray has a radiation dose significant enough to cause adverse effects on a developing embryo or foetus.
Some tips to make your dental visits comfortable
- Maintain healthy circulation by keeping your legs uncrossed while you sit in the dental chair
- Take a pillow to help keep you and the baby more comfortable
- Bring headphones and some of your favourite music

Can oral health have an effect on pregnancy?
There is increasing evidence supporting a link between gum disease and premature, underweight births. Pregnant women who have gum disease may be more likely to have a baby that is born too early and too small. More research is needed to confirm how dental diseases affect pregnancy outcomes.
Eating right for your teeth and baby
Although cravings for sugary snacks and treats are common during pregnancy, they should be avoided as much as possible. Keep in mind that the more frequently you snack, the greater the chances of developing tooth decay. Also, many studies have shown that the bacteria that cause cavities are passed from the mother to the child. Your baby's first teeth begin to develop about three months into pregnancy. Therefore, a healthy and balanced diet will ensure your baby has strong, healthy teeth. Well-balanced meals comprising dairy products such as cheese and yogurt are a good source of the essential minerals needed for a baby's developing teeth, gums, and bones.
After you have had your baby
If you had gum problems during your pregnancy, see your dentist as soon as possible after giving birth to have your entire mouth examined and your periodontal health evaluated.
Putting more focus on dental health and good oral hygiene habits during pregnancy will help both mother and child have healthy smiles for the rest of their lives.
Recent Blog Posts
- 28 Mar 2025
- 10 Nov 2023
- 19 Oct 2022
- 19 Oct 2022
- 19 Oct 2022
Fibroids and pregnancy
Fibroids and pregnancy
By Dr. Wee Horng Yen
Obstetrician and Gynaecologist
MB BCh BAO (Dublin), MRCOG (London), FAMS (Singapore)

What are fibroids?
Fibroids are non-cancerous tumours that grow in or around the womb (uterus) and are very common. The growths are made up of muscle and fibrous tissue and vary in size from under 1 cm to over 20 cm. Fibroids are sometimes known as uterine myomas or fibromyomas.
Many women are unaware that they have fibroids as they do not have any symptoms. This often means that fibroids are diagnosed by chance during a routine gynaecological examination, test, or scan.
However, larger fibroids may cause swelling in the lower tummy, pain, difficulty passing urine, a feeling of bulge while bending or constipation. If the fibroid impinges on the uterine cavity (the area where the baby grows), it may cause difficulty conceiving, miscarriage, or heavy and painful periods.
Fibroids that cause difficulties in conceiving require treatment. Surgery is the mainstay of treatment. Surgery can be performed using a keyhole or a traditional open (bikini line cut). If the fibroids are only in the uterine cavity, a hysteroscope can be used to remove them through the vaginal route without leaving any scars.
Patients whose fibroids are not too large may be offered keyhole surgery. Rarely in Singapore do patients present with fibroids that are very large, over 15 cm; occasionally a midline scar is needed for access to the tumour.
Keyhole surgery has the advantages of less pain, a shorter stay in hospital, and smaller scars.
After surgery, the surgeon will advise the patient on the duration of rest before they may conceive. This may be any time after three months post-surgery. Some patients will require a caesarean section for all future deliveries after fibroids are removed. This is to prevent rupture of the uterine scar during labour.
In the longer term, fibroids may recur, requiring future surgery.
Fibroids during pregnancy
One of the more common complications of large fibroids in pregnancy is “red degeneration”. This can cause moderate to severe pain and may be hard to tell apart from contractions of the uterus. When blood goes to the growing baby instead of the fibroid, red degeneration can happen. The reduction in blood and oxygen to the fibroid causes pain and the fibroids may shrink.
Rarely, fibroids within the uterine cavity may cause miscarriage. Very large fibroids may be associated with preterm birth. The majority of fibroids remain about the same size throughout pregnancy and do not cause major complications.
As long as the fibroid is not physically obstructing the passage of the baby, women with fibroids may undergo natural birth.
Fibroids noted at caesarean section
It is not routine to remove fibroids at caesarean delivery. This is because of the increased risk of bleeding in doing so. The exception is when the fibroids are “sticking out” or at the surface. In these cases, the base of the fibroid is much smaller and it may be safely removed.
Recent Blog Posts
- 28 Mar 2025
- 10 Nov 2023
- 19 Oct 2022
- 19 Oct 2022
- 19 Oct 2022
Pagination
- Previous page
- Page 2
- Next page
