Antenatal screening tests for chromosomal abnormalities
Antenatal screening tests for chromosomal abnormalities
By Dr. Loke Kah Leong
MBBS (S'pore), MMed (O&G), MRCOG (UK), FAMS (S'pore), FICS (USA), FRCOG (UK)

There are a few screening tests for chromosomal abnormalities that are available and are offered to all pregnant women in the late first trimester or early second trimester. These include the nuchal translucency (NT) scan, the NT combined with a maternal blood test, commonly known as the OSCAR test or maternal serum screening test (e.g., Triple Test).
Screening tests are all non-invasive and there is no risk of causing miscarriage. Since the chance of chromosomal problems goes up as a woman gets older, screening tests are even more important now that more women are having babies later in life.

Nuchal translucency (NT)

The NT test involves a detailed ultrasound scan of the baby at 11–14 weeks of gestation, and the fluid collection behind the baby’s neck is measured. A thickened NT beyond normal thickness is associated with chromosomal abnormalities, Down’s syndrome being the most common, although Edwards’s syndrome and Patau’s syndrome are also screened. The normal thickens is usually less than 2.5mm.
A risk estimate can be obtained by the foetal NT value, maternal age, and the crown-rump length of the fetus. The accuracy of the NT test alone is about 80%.
OSCAR
The OSCAR test involves the NT test plus a sample of the mother’s blood, which is analysed for levels of free beta hCG and PAPP-A (pregnancy associated plasma protein A). The combined data will give a risk estimate of Down syndrome with an accuracy of 90% which is superior to that NT alone (80%)
Maternal serum screening
The maternal serum screening test is done between 15–20 weeks of gestation and this measures certain hormones in the blood to determine risk. The triple test measures three hormones called alpha-fetoprotein, human chorionic gonadotrophin, and oestriol, and a risk value is calculated according to maternal age and the gestational age of the fetus at that time.
As its accuracy is only 65%, this test is less commonly done nowadays. Furthermore, it has to be done later from 15 weeks onwards compared to NT and OSCAR, which can be done from 11 weeks onwards.
Interpretation of the results

The result of the screening test will give you a numerical risk value, which tells you if your fetus belongs to a low-risk or a high-risk group. Screening tests are not diagnostic tests and cannot tell you if your baby has Down’s syndrome.
A result of 1 in 300 means that one in 300 women will have an affected baby. Similarly, it also means that 299 out of 300 women with these results will not have an affected baby.
From a medical standpoint, the cut-off point between high and low risk is taken at 1:300. Therefore, 1:50 would be considered high risk and 1:1000 would be low risk. It is important to understand clearly that the results of screening tests represent risks.
Even if the risk is low, there is still a chance that the baby could have Down's syndrome or another abnormality. Conversely, a high-risk result does not mean the fetus is affected and further diagnostic invasive tests (e.g., chorionic villus sampling or amniocentesis) must be done.
Invasive tests obtain cell samples from the foetus, and the results will be able to confirm if the baby is affected by Down’s syndrome. The risk of miscarriage related to the procedure is 0.5%. A normal result would undoubtedly give the parents peace of mind, whereas an abnormal result would give the parents the option of continuing the pregnancy or terminating it.
Recent Blog Posts
- 28 Mar 2025
- 10 Nov 2023
- 19 Oct 2022
- 19 Oct 2022
- 19 Oct 2022
Non-invasive prenatal testing (NIPT)
Non-invasive prenatal testing (NIPT)
by Dr. Francisco M. Gil-Salas
PhD, MSc, B. Pharm

Prenatal testing is an essential step in providing security. It ensures that you stay informed about the status of your pregnancy. Aside from reducing anxiety and stress, it gives you peace of mind and also an expectation of what’s in store for the journey ahead, so that you are able to provide the best start for your child.
The detection rates of conventional screening tests currently available vary from less than 70% to a high of 84%, implying that 16% to 30% of abnormal fetuses are potentially missed during screening. Also, these traditional screening methods have a false-positive rate of 5%. This means that 1 in 20 women who go through screening will have to go through an unnecessary invasive test.
Since the groundbreaking discovery of cell-free DNA (cfDNA) in the blood of pregnant women in 1997, it has given non-invasive prenatal testing (NIPT) new ways to check on a baby's health. NIPT has been increasingly used as a screening test to detect foetal chromosome abnormalities. The cutting-edge Next Generation Sequencing (NGS) technology is used to look at the cell-free DNA in the mother's blood. This cfDNA comes from the placenta and circulates freely in the maternal bloodstream. The risk of aneuploidies like Down Syndrome is found by looking at millions of reads of sequencing data from this cfDNA. This can be done with up to 99% accuracy.
The whole genome sequencing approach based on NIPT provides comprehensive coverage for chromosome abnormalities. Such a test can be performed as early as 10 weeks of gestation, although waiting till 12 weeks is recommended when the pregnancy is more stable. It could be seen as a supplement to an ultrasound evaluation in the first trimester and a nuchal translucency scan (NT Scan). Expectant mothers include women with any of the following conditions:
- Advanced maternal age (Over 35)
- Abnormal maternal serum screen
- Abnormal ultrasound findings suggestive of fetal trisomy
- High and intermediate Risk” in First Trimester Screen
- Family history of chromosomal abnormalities
NIPT is a highly accurate screening test, but it is not a diagnostic test. It does not test for all chromosomal conditions. So, a "screen negative" result does not completely rule out all fetal chromosomal disorders that were not tested. Confirmatory testing, appropriate follow-up obstetric care, and counseling are strongly recommended for women who are identified as being at high or elevated risk.
Recent Blog Posts
- 28 Mar 2025
- 10 Nov 2023
- 19 Oct 2022
- 19 Oct 2022
- 19 Oct 2022
Prenatal tests – what can you expect?
Prenatal tests – what can you expect?
To all the parents-to-be, congratulations on your bundle of joy! These upcoming months are going to be an amazing journey for you and your other half. We know that all parents want to be as ready as possible for their baby, so here's a quick rundown of the different prenatal tests you can expect and talk about with your OBGYN doctor.
What are prenatal tests?
Prenatal tests are medical tests you get during pregnancy. These are tests to check the mother’s and her baby’s health. With the help of modern science, you can find out if a baby is at risk for problems like preterm birth, chromosomal abnormalities, and foetal abnormalities.
Basically, there are two types of prenatal tests:
- Screening tests
These tests are a gauge to identify whether a condition is present in your baby. It does not give a definite answer, and is often used as an indicator. A few examples of prenatal screening tests are blood tests and specific types of ultrasound. - Diagnostic tests
Prenatal diagnostic testing will give you an accurate diagnosis to whether your little one might carry certain health conditions. However, these are invasive and are only recommended when a screening test shows indication of a disorder.
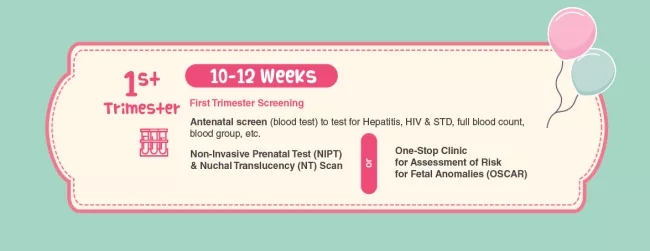
1st Trimester
In your first trimester, you should focus on antenatal screening tests. It helps to screen for chromosomal abnormalities, hepatitis, sexual transmitted diseases and many more. These screening tests are non-invasive and will not cause any miscarriage risk to the pregnancy.
Also, because women are having babies later in life, prenatal screening tests are more important than ever.1 As maternal age rises, the risk of chromosomal abnormalities increases as well. Early detection for your little one is important, and many mommies-to-be are encouraged to take these tests to get a better understanding of the future.
There are two available options for testing chromosomal abnormalities:
Remember to consult your OBGYN doctor and do your research before taking any of these tests.
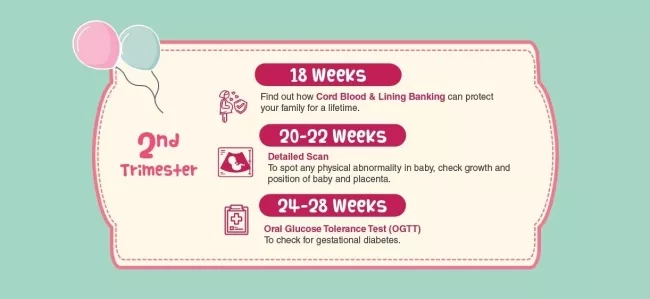
2nd Trimester
In the course of your second trimester, your baby’s organs have become more developed, and towards the end of your second trimester, your baby starts to get active. Mommies-to-be will begin to feel the joy of your little one moving around and kicking.
During this period, an important service to consider is cord blood and cord lining banking. Get educated on how stem cells play a part in being biological insurance for your family and how the collection process by your OBGYN doctor is painless, simple, and risk-free. As the umbilical cord stem cells can only be collected at birth, do take some time to understand this more.
Week 20 to 28 of your pregnancy is when you should go for your detailed scanning and oral glucose tolerance test (OGTT).
- Detailed scanning
A second trimester detailed scan is an ultrasound scan which allows the doctor to check your baby’s body structure. It’s used to spot any physical abnormalities, check growth, the position of your baby and the placenta. Ultimately, this scan helps to prepare you and your doctor for the delivery and care of your little one after birth. - Oral glucose tolerance test (OGTT)
An OGTT is simply a test that measures how well your body responds to glucose after you consume a specific amount of sugar. Firstly, you will have to fast overnight. On the day of your OGTT, a blood sample will be taken from you on an empty-stomach. This will determine your glucose level when you are fasting. You will then need to drink a glucose solution given by the nurse. Your blood samples will be taken after 1 and 2 hours after you consuming the solution. This test ultimately diagnose whether you might have gestational diabetes mellitus (GDM).

3rd Trimester
In your third trimester, it is soon to be a home run for you! We understand that you may feel even more uncomfortable due to the weight gained, sleepless nights and might go through labour contractions that are false (also known as Braxton-Hicks). Our piece of encouragement is to hang in there, mommies-to-be. You will see your little one very soon, and good job so far.
The tests that will be required are the whooping cough vaccine and group B strep.
- Whooping cough vaccine
It’s strongly encouraged by many for pregnant mothers to undergo the whooping cough vaccine. The purpose of this vaccine is to prevent you and your baby from contracting tetanus, diphtheria and pertussis (Tdap). These illnesses are highly contagious and therefore it’s important to get vaccinated to protect your baby. - Group B strep test
What is Group B streptococcus you may ask? It is a type of bacteria that is found in the vagina or the rectum in 30% to 40% of women.2 The concern rises when the bacteria has been passed on to your little one through normal delivery. The infection usually manifests in a form of pneumonia or meningitis in your child.
This information may seem very serious. Fret not, there is a test to see if mommies are carriers of this bacteria. If they happen to be tested positive, they can be treated with doses of antibiotics to reduce the chances of passing it to your baby.
To all the parents-to-be, these are just nuggets of information to better prepare you for your pregnancy journey. Always remember to consult your OBGYN doctor to understand what other details you might need before performing any tests.
References:
1Strategy Group Singapore. (2011). Marriage and Parenthood Trends in Singapore. https://www.strategygroup.gov.sg/images/Press%20Release%20images/PDFs/marriage-and-parenthood-trends-in-singapore.pdf
2Vaginal Discharge During Pregnancy. (2019, August 9). Retrieved July 29, 2020, from https://www.healthhub.sg/live-healthy/993/pregnancy-vaginal-discharge-during-pregnancy
Recent Blog Posts
- 28 Mar 2025
- 10 Nov 2023
- 19 Oct 2022
- 19 Oct 2022
- 19 Oct 2022
